Understand how overwhelming it can be to face a diagnosis of gastrointestinal (GI) cancer. Whether it’s colon cancer, stomach cancer, pancreatic cancer, or any other form of GI cancer, one of the most important steps towards recovery is getting the right surgical treatment.
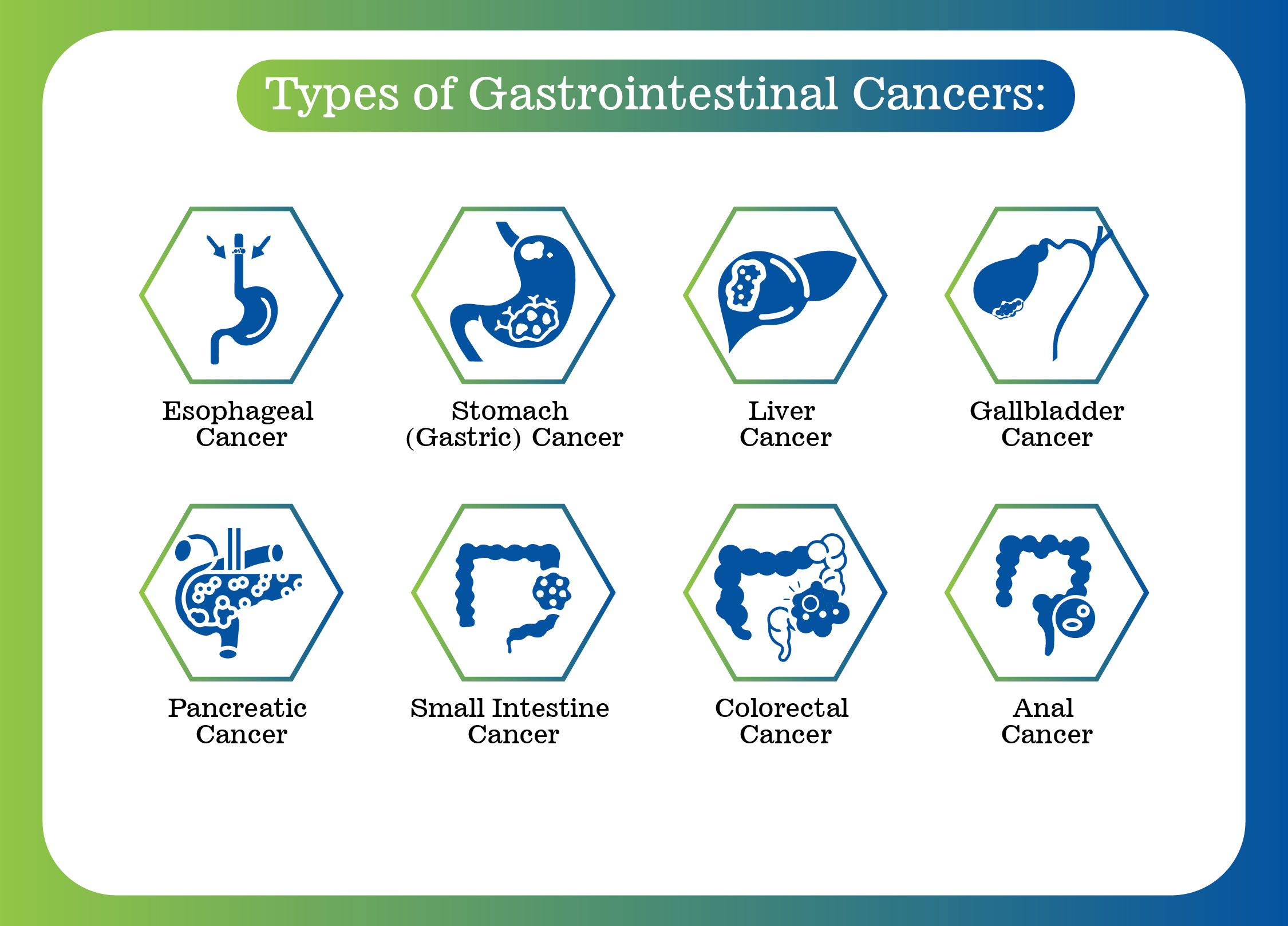
Gastrointestinal cancer refers to cancers that affect the digestive system. This includes organs like:
Each type of GI cancer is unique, requiring specialized care and treatment. Surgery is often one of the most effective ways to treat GI cancers, especially when the cancer is detected early and hasn’t spread too far.

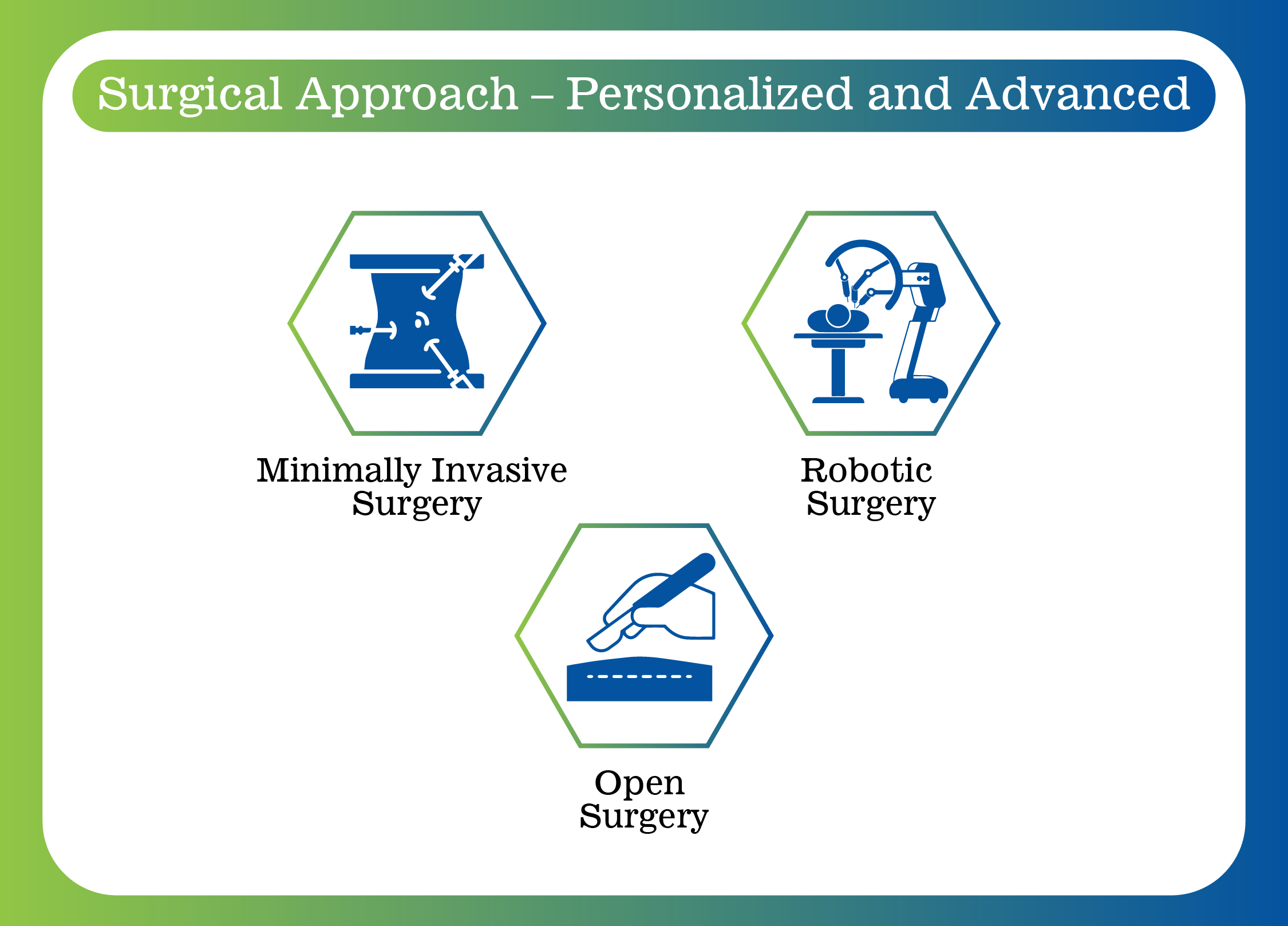
Understand how overwhelming it can be to face a diagnosis of Surgery is one of the most effective treatments for many GI cancers, especially when the cancer is localized and hasn't spread. It aims to:
Depending on your case, surgery might be combined with other treatments like chemotherapy, radiation therapy, or targeted therapy for the best outcomes.
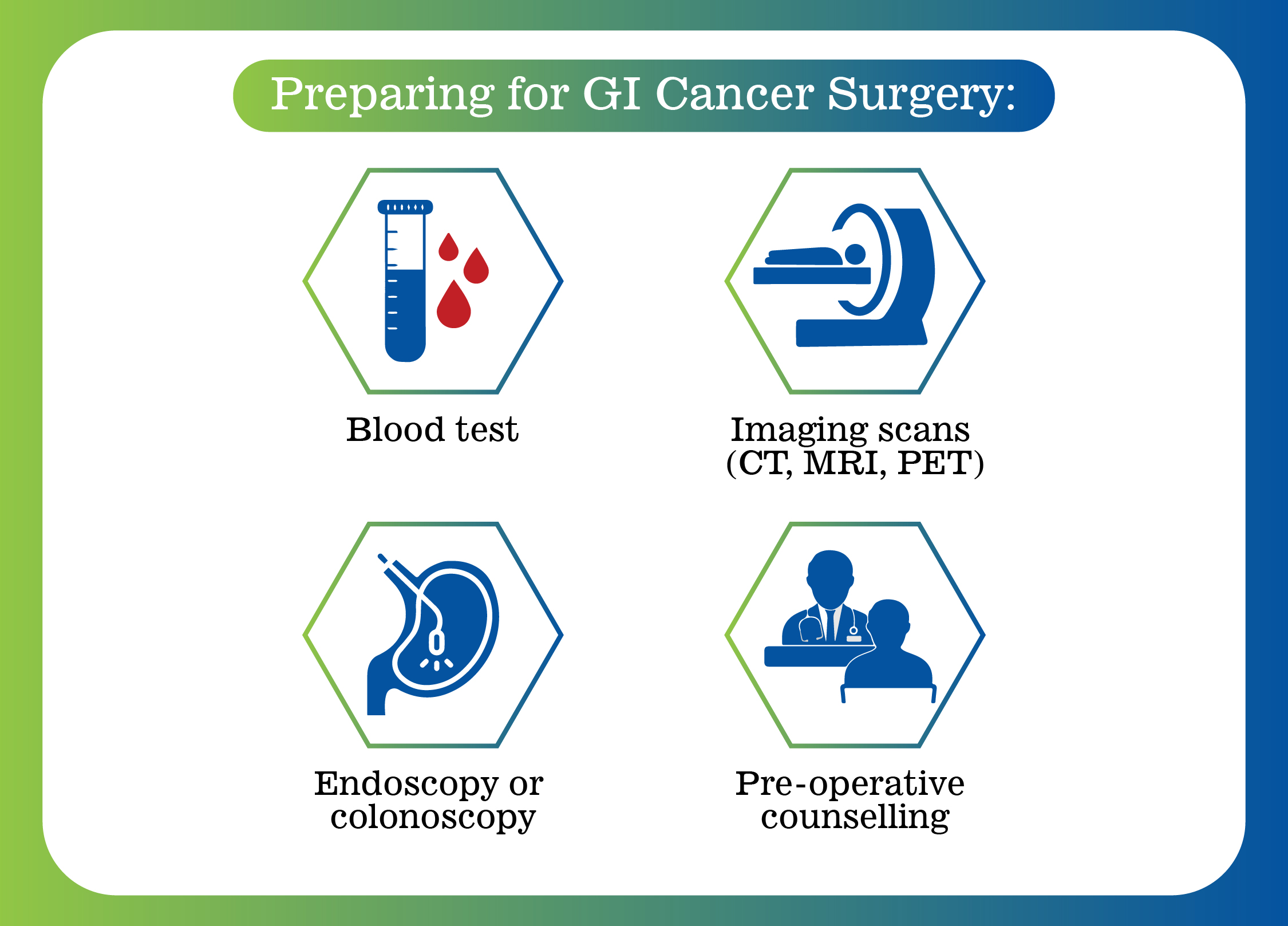
Before your surgery, our team will conduct a complete evaluation to ensure you’re ready for the procedure. This may include:
We also provide nutritional guidance, mental health support, and help with managing any pre- existing conditions to optimize your health before surgery.
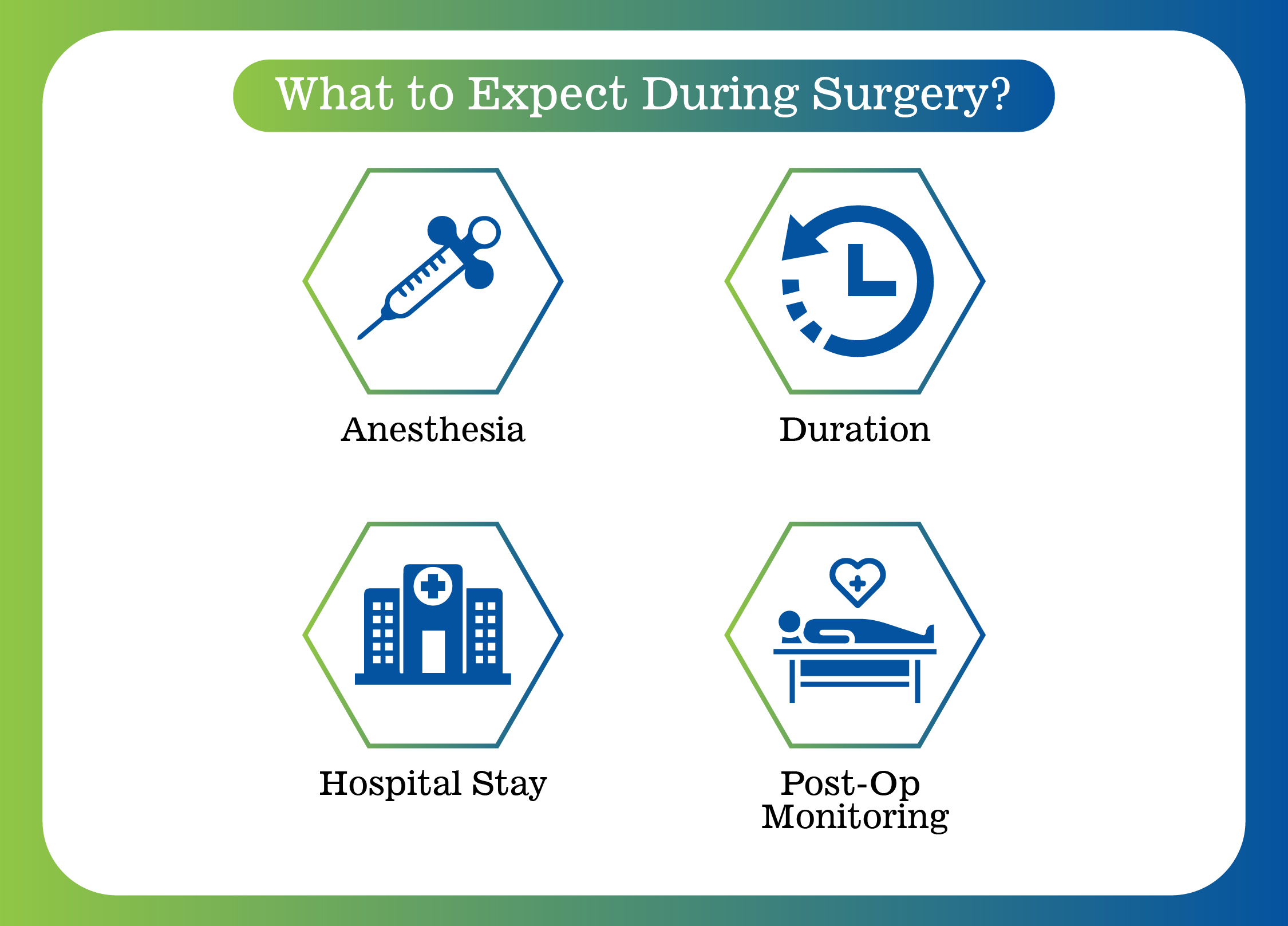
Each type of gastrointestinal cancer surgery is different, but here’s a general overview of what you can expect:

Recovery time varies depending on the type of surgery and your overall health. Here’s what recovery typically involves:
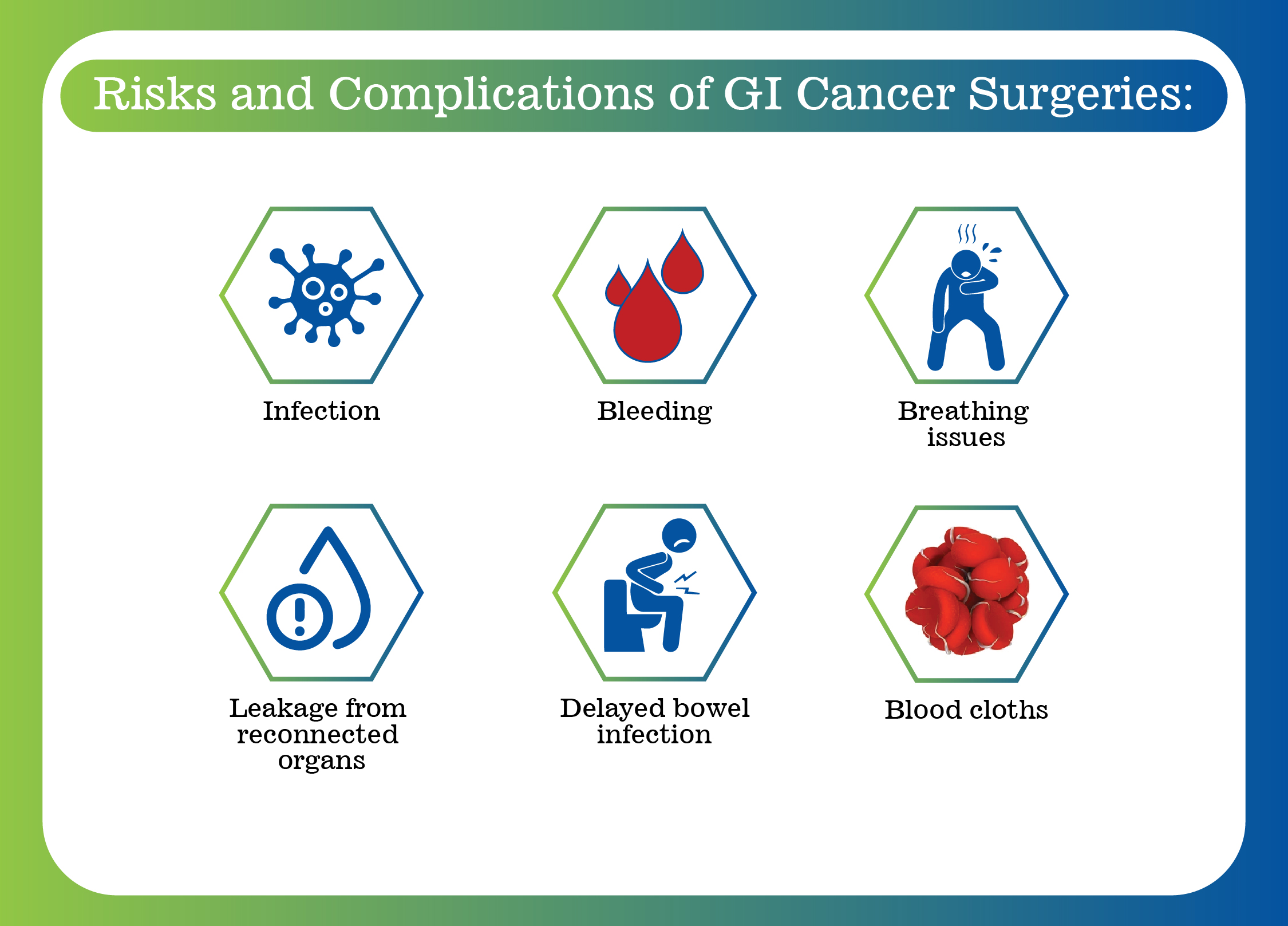
Like any surgery, GI cancer surgeries come with certain risks, including:
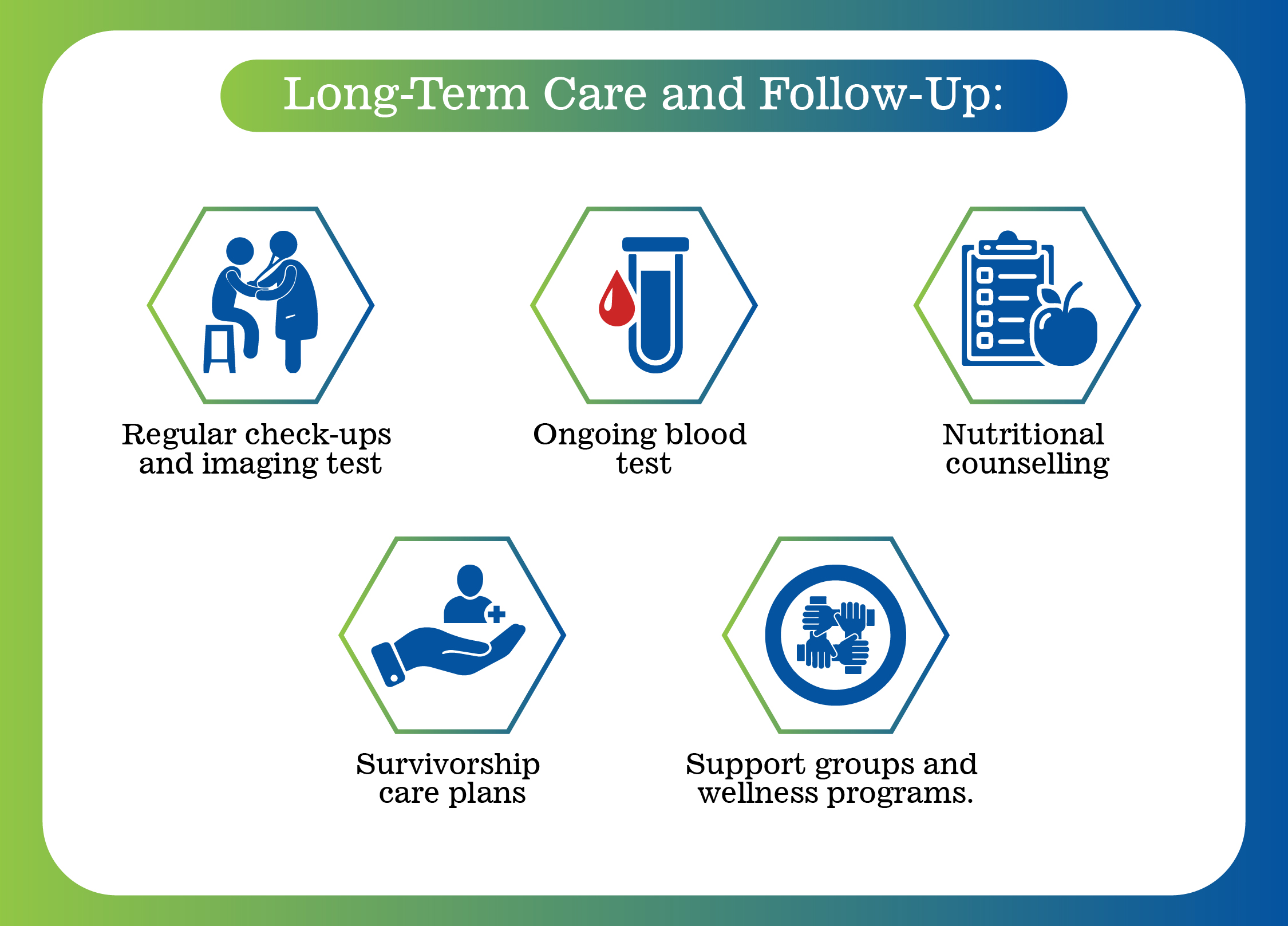
Surgery is just one part of the journey. Long-term follow-up is critical to check for recurrence and maintain your health.