The pancreas is a small but mighty organ in your abdomen that plays a crucial role in digestion and blood sugar control. When something goes wrong—such as a tumor, cyst, or chronic inflammation—surgery may be the best treatment option.
Before diving into surgeries, let’s understand the pancreas.
The
pancreas is a flat, fish-shaped organ located behind your stomach. It
performs two essential
functions:
When the pancreas becomes diseased—due to cancer, cysts, chronic pancreatitis, or trauma—it can severely impact your digestion and overall health. That’s when surgery might become necessary.
Depending on the condition, your surgeon may recommend one of the following procedures. Each is designed to remove the affected area while preserving as much pancreatic function as possible:
The digestive tract is then reconstructed to allow normal digestion. Although complex, this surgery offers significantly improved outcomes when performed by experienced surgeons.
Not every pancreatic issue requires surgery, but in certain cases, it becomes essential. Common reasons include:
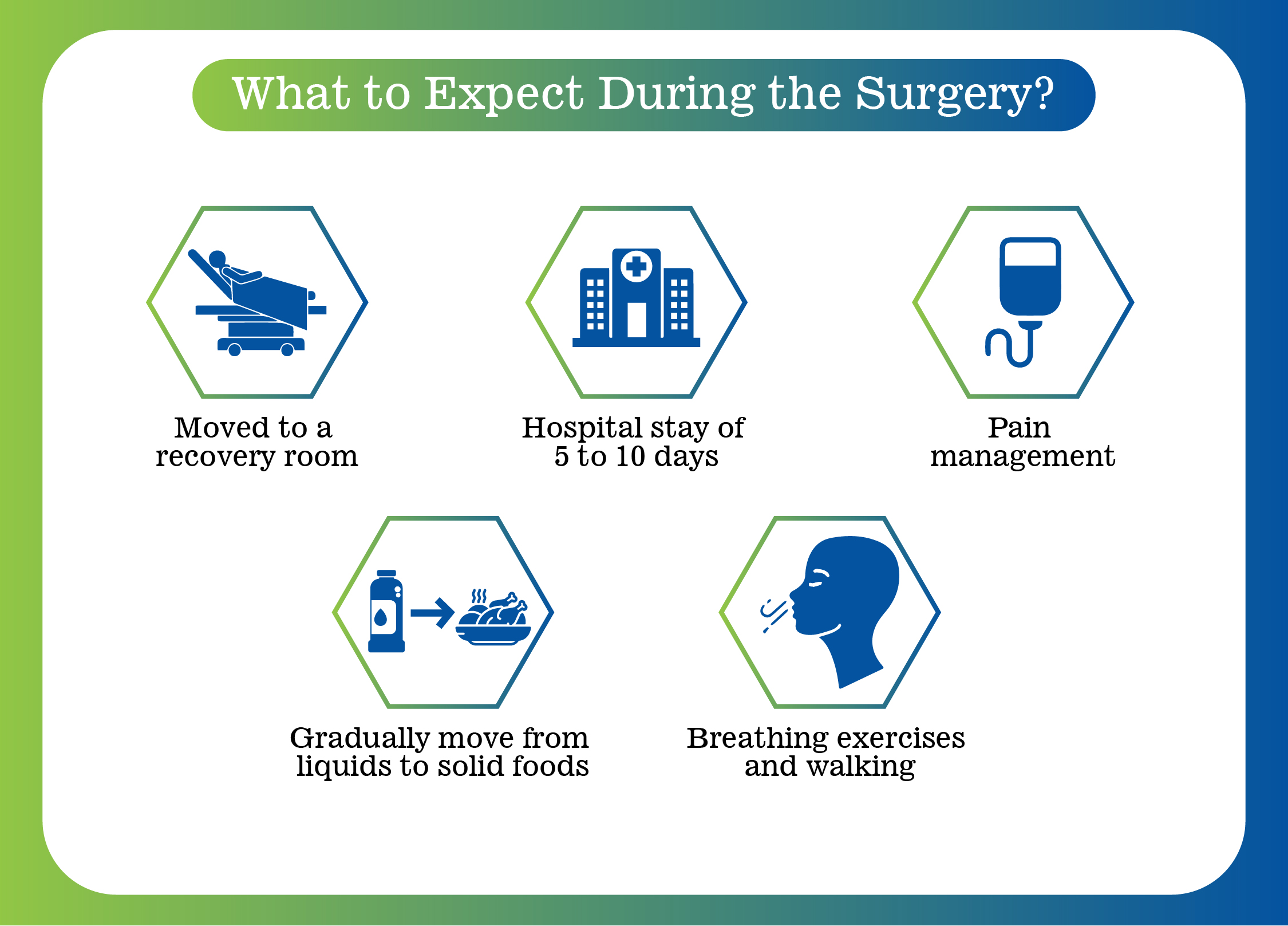
Pancreatic surgery is typically performed under general anesthesia and may take several hours. After surgery:
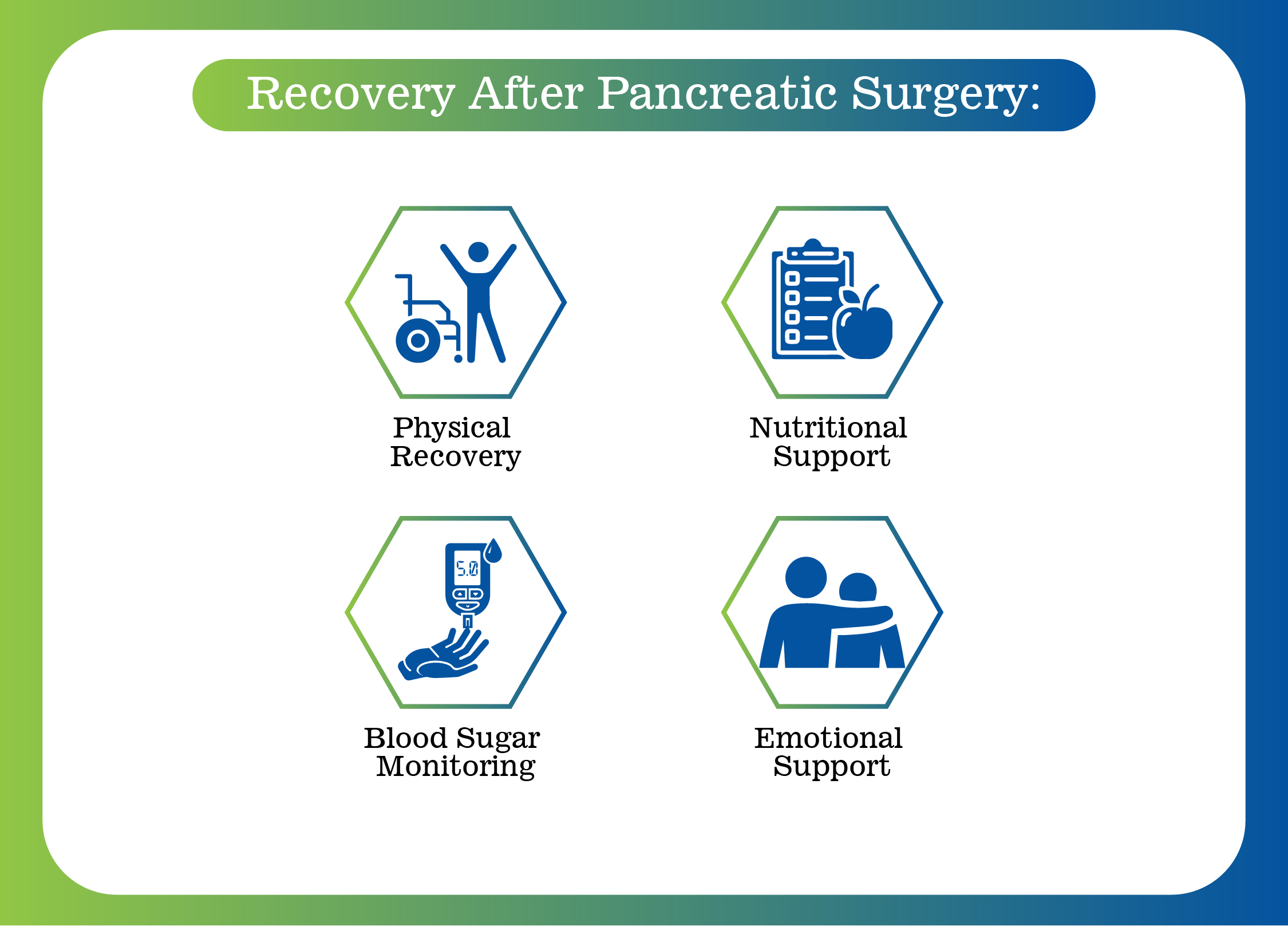
Recovery continues at home and marks the start of a new phase in healing.
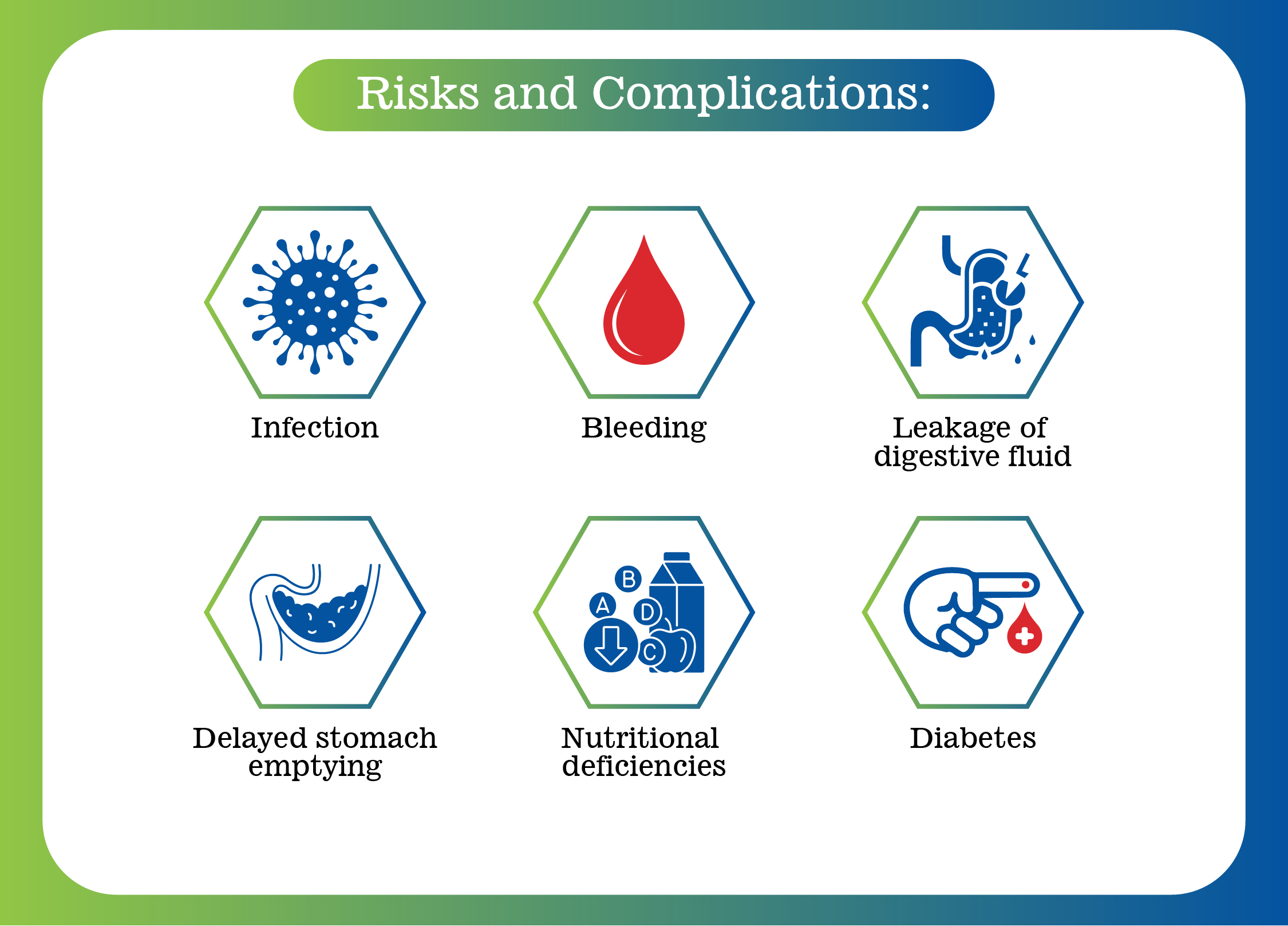
Like any surgery, pancreatic surgery carries risks, including:
Being aware of these risks and having a good surgical team helps in managing them effectively.
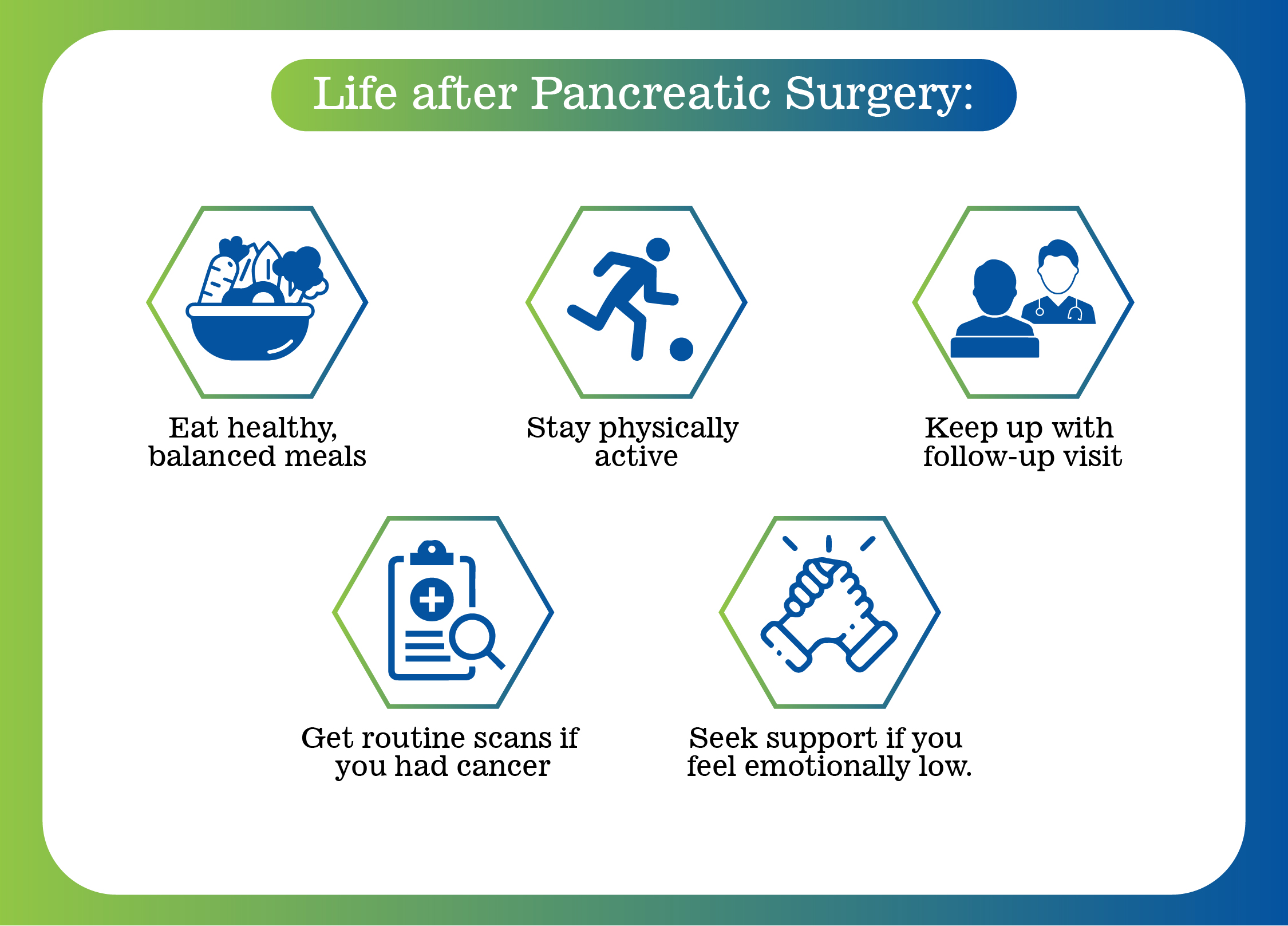
Life may feel different after surgery, but it is far from over. With the
right support, most patients
return to their routines and lead fulfilling lives.
You’ll be encouraged to:
Pancreatic surgery may sound overwhelming, but for many, it offers hope, relief, and even a cure. Whether it’s for a tumor, cyst, or chronic inflammation, these surgeries are powerful tools for improving quality of life.
Thanks to advances in surgical techniques and the expertise of dedicated specialists, outcomes are now safer and more successful than ever. With the right medical care, nutritional guidance, and follow-up, you can look forward to a healthier future.